By Cindy Moffett | Portrait photos by Tyler Oxendine
In 2015, the U.S. Centers for Disease Control ranked Tennessee’s Campbell County third in the nation for opioids prescribed per capita.
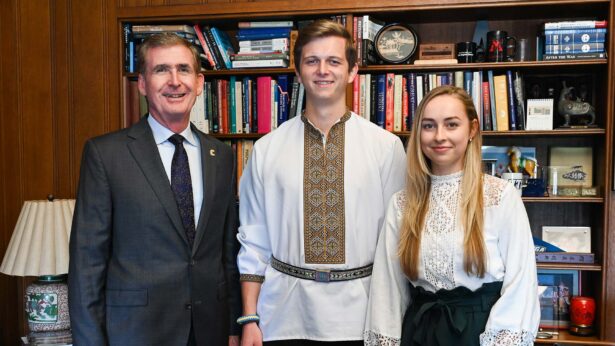
That wasn’t the future Dr. Geogy Thomas, Knoxville ’15, envisioned 18 years ago when he moved to tiny Jellico, located in Campbell County near the Kentucky border. Fresh out of medical training in California, he had planned to be a missionary overseas with his wife. First, though, they detoured to Jellico to pay off his student loans through two years of medical service to an underserved community.
“We fell in love with this place, these mountains and, especially, its people,” Thomas says. “It was a different kind of need than being overseas, but it was exactly what we were called and designed to do.”
As a family physician, Thomas joined Dayspring Family Health Center, which cares for people from birth to death in the former coal-mining area. Early on, he was surprised by a difference between his California and Tennessee patients.
“A lot of people here liked their prescription drugs. It was for back pain, it was for nerve pills, and it was all much more than I had seen before. I said no and went toe-to-toe with a lot of people,” Thomas says.
Campbell County, Tennessee
In 2015, the U.S. Centers for Disease Control ranked Campbell County third in the nation for opioids prescribed per capita using morphine mg equivalents.
2017 population: 39,771
Number of Patients Receiving Opioids for Pain
2013: 13,905
2014: 13,428
2015: 13,116
2016: 12,580
2017: 11,587
Total Morphine Milligram Equivalents for Opioids Per Capita
2013: 3,284.1
2014: 3,102.8
2015: 2,903.5
2016: 2,497.1
2017: 2,477.0
Number of Opioids for Pain Prescriptions
2013: 83,004
2014: 82,882
2015: 82,498
2016: 77,114
2017: 71,399
Number of Patients Receiving Buprenorphine for Medication Assisted Treatment
2013: 564
2014: 815
2015: 966
2016: 790
2017: 786
(Tennessee Department of Health)
There were other sources of drugs, though, such as from Tennessee’s then-proliferating pill mills, where powerful narcotics were prescribed liberally. When patients later returned to Dayspring, some would be taking three or four times the originally prescribed pain medicine.
For more than 20 years, opioids spread their tentacles throughout the nation. Marketed as safer than previous painkillers and nonaddictive, prescription drugs such as Percocet and Vicodin became widely prescribed. However, the marketing proved false. The drugs ensnared patients in addiction.
“We have seen the impact of this opioid epidemic in our community,” Thomas says. “Socially, physically and emotionally, families are just destroyed. You go through our little town, and you see brokenness—people who are struggling, down and out.”
Melissa Hamby, care manager for Dayspring Family Health Center, knows when the crisis hit Jellico in force.
“2010 is when the floodgates opened,” she says. “That’s when we had to change how we did obstetrics care and start screening the moms for drugs.”
Opioids take a toll on the most innocent. Addicted mothers deliver addicted babies. Those babies are diagnosed with neonatal abstinence syndrome (NAS), a wrenching drug-withdrawal process that necessitates hospital stays of four to six weeks for the newborns. From fevers to rapid breathing, seizures to inconsolability, the infants suffer.
Initially, Thomas sent addicted mothers to High Risk Obstetrical Consultants at UT’s Medical Center. Eventually, though, he learned that many referred patients never made it to Knoxville. “Some of those moms stopped getting care or they went, but returned to deliver with us anyway,” he says.
Thomas looked for ways to support the women closer to home. Dr. Craig Towers of Obstetrical Consultants was exploring the detox of pregnant women—a new concept—through weaning doses of buprenorphine, an opioid replacement drug. Patients are gradually moved to the lowest possible dose and, eventually, if possible, to none at all. In consultation with him, Thomas and his obstretics partner, Dr. Cathleen Suto, began treating their patients.

“But the more we worked,” Thomas says, “the more we understood that it’s not just a matter of taking them off the drugs. It required us helping them reset their lifestyle, establish a new friend group and adopt new coping skills. What we learned is that the whole drug was quite intricate and quite consuming.
“Many of our patients returned pregnant the next year. And still on drugs. We may have gotten them off drugs, but, unfortunately, they returned to homes that were broken, to partners or parents who abuse drugs. So we had to figure out not just how to take care of that one patient in the room and the baby in that womb but the whole family unit.”
To broaden his skills, Thomas earned a Physician Executive MBA from UT Knoxville’s Haslam College of Business. While there, he studied how to open a comprehensive detox program in Jellico. He hoped to create an inpatient program at the local hospital, but that turned out to be more than the small hospital could undertake. Dayspring created an outpatient program instead.
“Our vision was to restore hope and reclaim the future,” Thomas says.
It began with Suto.
“Dr. Suto is a pioneer,” says Thomas. “She started our outpatient MAT program—medication assisted therapy—for pregnant women. Dr. Suto also helped develop our behavioral health program. These women meet weekly as a group with a counselor, learning from their struggles as they gradually come off drugs, helping them reclaim their lives.”
Hamby, who worked as a nurse with Dayspring for 13 years, joined the MAT program in October 2017. She gathers histories, manages paperwork and appointments, and smooths program interaction for the patients. About 40 patients are in the MAT program, and about 18 women are in support groups. The program lasts for a minimum of 20 weeks; after that, the length varies according to the individual’s needs.
| Year | Number of Cases | Percentage of Live Births |
|---|---|---|
| 2013 | 935 | 1.17 percent |
| 2014 | 1,034 | 1.27 percent |
| 2015 | 1,049 | 1.29 percent |
| 2016 | 1,071 | 1.33 percent |
| 2017 | 1,090 | 1.35 percent |
(Tennessee Department of Health)
| Healthy Infants | NAS Infants | |
|---|---|---|
| Average cost: | $8,494 | $44,314 |
| Average hospital stay: | 3.5 days | 21 days |
(Tennessee Department of Health)
The outpatient program tries to remove as many barriers to treatment as possible.
“Even the stigma of having your car sitting at a detox or rehab clinic can be enough to make some people say no,” Thomas says. “By providing such a comprehensive service in a patient’s medical home, they are more likely to pursue and succeed at treatment. Our patients can see their counselor and their primary care doctor in one sitting. At the same time, our care managers are available to get our patients resources they need such as insurance, housing, food, or even safety from abusive relationships.
“We want to care for the whole person. Addiction affects every part of your existence: Your family, your psyche, your spiritual, physical, financial health—it hits everything. If a clinic’s not prepared to address those issues, healing is not possible and definitely not sustainable.”
Clients have been motivated to move through the difficult journey. “Most have young children, and they want to make their families complete,” Hamby says.
“I didn’t want my baby born addicted,” one program graduate says. “I wanted to do better for myself and him. Recovery is tough, and other ways don’t work. You need the support group and education to do better.”
She participated in the program through pregnancy and for several months after delivery. “My baby is doing OK,” she says proudly. “He didn’t have any withdrawals.”
She recommends the program to anyone needing help. “The people at Dayspring are supportive. They listen and don’t judge. A lot of doctors judge you.”
While Suto works with the MAT women, Thomas works with the men. “They’ve hit rock bottom,” he says. “They’re saying, ‘I’m ready, more than ready. Help me get off this stuff.’ If you can give them the care they need at that moment, it’s gold. We’ve seen men get jobs, be reunited with their kids and wives. We’ve seen men that were spending $150 a day on drugs cleaned up and leading more purposeful lives.” He hopes to create a support group for men in the future.
For Thomas and the committed staff at the Dayspring Family Health Center, these comprehensive programs are a way to rebuild the community. “We’re on a mission to make a difference and restore our community, one patient at a time. The spirit of Appalachia is its people—strong, good people. That’s all the reason to fight to keep our community alive.”
The Next Wave
Even as Dr. Geogy Thomas works to combat the opioid crisis, he’s preparing for the next, related crisis: hepatitis C.
Hepatitis C, a virus, is prevalent in drug users. It is easily contracted from drug paraphernalia—needles, snorting straws—and can live on surfaces for weeks, posing a threat to any bloodstream it enters—family members, children, the elderly.
The virus can lie dormant for 10 to 15 years before revealing itself through liver failure. “We’ve been screening our obstetric patients for the past five years, and our rate of infection is almost 12 percent. The national obstetric average is 1.5 percent,” Thomas says. “Hepatitis C is curable, but the drugs and treatment are very expensive.”
Thomas said the clinic is working to install the equipment to begin treating infected patients by January 2019.